Remdesivir, a vial for 100 ml water solution with 100 mg effective substance to be diluted with physiological solution. Gilead Sciences, 2020. NML Medical Museum, 309/2020. Photograph by Tereza Vobecká
Object of the Month: July 2020
Remdesivir
A collection of objects that depicts life in the time of a pandemic must include medicines. In a story of fighting disease, a drug bottle or phial represents victory, prefigures the end of the hard times and gives face to the hope that defeating the plague is in human power and within reach. If face masks came to symbolize the common struggle with the coronavirus on the one hand and the constraints of state power during emergency on the other, medicines stand for the trust in science and scientists, competent and qualified to protect us all. Controversies over the effect of particular chemicals, negotiations over the price of medicines or the aspirations of politicians to secure or to limit access to remedies show, at the same time, the context in which science is done and the extent to which our trust is justified.

Favipravir, an antivirotic developed in Japan, appears to be effective against COVID-11 as well. NML Medical Museum, 76/2020. Photograph by Veronika Löblová
During the COVID 19 pandemic, up to 540 drugs have been tested for their power to act against the disease. Besides antivirotics, preparations that directly restrain transcription and replication of the virus, promising medications include anti-inflammatory drugs, anticoagulants that prevent blood clots, preventing respiratory failure and reducing mortality, interferons that stimulate the immune response of the body, or the blood plasma of recovered patients with sufficient levels of SARS-CoV-2 virus antibodies. All potential remedies remain experimental at this point. Some – such as the antimalarial drug hydrochloroquine of the combination of antivirotics lopinavir and ritonavir – have been found wanting: clinical tests of dozens of others continue.
Remdesivir, a broad-spectrum antivirotic developed by the team led by dr. Tomáš Cihlář (1967-) in the Gilead Sciences Company, belongs to the most promising compounds directly affecting the virus. The drug was originally developed to treat viral hepatitis C and infections caused by the respiratory syncytial virus (RSV). During Ebola epidemics in Western Africa (2014, 2016-2018) it was clinically tested and provided, in the framework of compassionate use, to a few severely ill patients in the Democratic Republic of Congo. Further research in 2014-2018 investigated the effect of the compound against SARS and MERS viral respiratory infections. Clinical testing of remdesivir as a cure for COVIS-19 begun in Beijing in February 2020; at the same time, it was made available to the first COVID-19 patients in the United States. The drug turned out significantly to shorten recovery times in patients with lower respiratory infection associated with the SARS-CoV-2 virus. Early application of remdesivir enhanced its benefit.
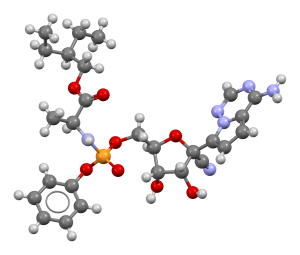
Remdesivir is administered by intravenous infusion, starting with a 200 mg loading dose on the first day and following with daily maintenance dose of 100 mg for up to 10 days. The compound is metabolized into remdesivirtriphoshate (RemTP), whose molecule resembles (constitutes and analog of) adenosine triphosphate (ATP), substance required by the viral enzyme RdRP (RNA- replicase) as energy source for replicating generic information of the viral RNA. RemTP binds to the RdRp, taking the place of ATP and blocking the action of the RdRP and thus the reproduction of the virus in the cell.)
The Czech Republic requested the supply of remdesivir on March 16, 2020, and on the following day, permission was granted by the State Institute for Drug Control (SÚKL). On March 24, the drug was administered to the first patient with COVID-19 associated pneumonia at the Clinic of Anesthesiology, Resuscitation and Intensive Medicine (KARIM) of the Prague General Faculty Hospital. In early May, the patient was released to home care. In April, COVID-19 patients at the Motol Faculty Hospital KARIM Clinic and the III. Clinic of Infectious and Tropical Diseases of the Bulovka Hospital in Prague and in May, at the Clinic of Anesthesiology and Resuscitation of the St. Anne’s University Hospital in Brno received the medication as well.
Remdesivir is intended for patients with severe respiratory infections, in need of artificial lung ventilation, and its administration depends on extraordinary permissions. No COVID-19 medication has so far passed the necessary certification and approval procedures for regular use, whether in the Czech Republic, the European Union or the United States. Voices of doubt and critical stances are a necessary part of the scientific debate on the benefits of any medication. The improvement of COVID-19 patients treated by remdesivir is, however, likely linked to the effect of the drug and the latter’s side-effects are relatively minor. From a practical, as well as an ethical viewpoint, it is impossible to withhold such medication, once available, from patients in life-threatening conditions.
The frightening advance of the global pandemic has animated the desire for a “magic bullet” targeting the virus, an effective and safe cure that would remove the

One of the first promising “magical bullets,” Neosalvarsan (1912). Neosalvarsan found use in the treatment of the Spanish Flu Pandemic in 1818-1920 as well.
NML Medical Museum Pharmacy Collection, PH 345. Photograph by Tereza Vobecká
disease from the world. We have no such weapon and we are not likely to find one. Recovery from COVID-19 is the result of complex hospital care that includes respiratory support as well as a combination of medicines affecting both the agent and the symptoms of the disease. The end of the pandemic – when, and if, it is over – will require new medications, but also effective treatment procedures, daily exertion of physicians, nurses and other medical professionals, as well as continuing preventive measures and the consideration of both the healthy and the ill for all others living with the shared danger. Without hope and trust – represented here by a small bottle that contained a possible cure – we can attain none of that.
We are grateful to Associate Professor MUDr. Tomáš Vymazal, CSc., MHA, Head of the KARIM Clinic of the Charles University Second Faculty of Medicine and the Motol Faculty Hospital, MUDr. Jan Beroušek, Head Physician of the Inpatient Unit, KARIM, Motol Faculty Hospital, as well as Associate Professor MUDr. Hanuš Rozsypal, CSc., Head of the Clinic of Infectious, Parasitic and Tropical Diseases, Bulovka Hospital, for their interest in our collections and their significant contribution to their growth.